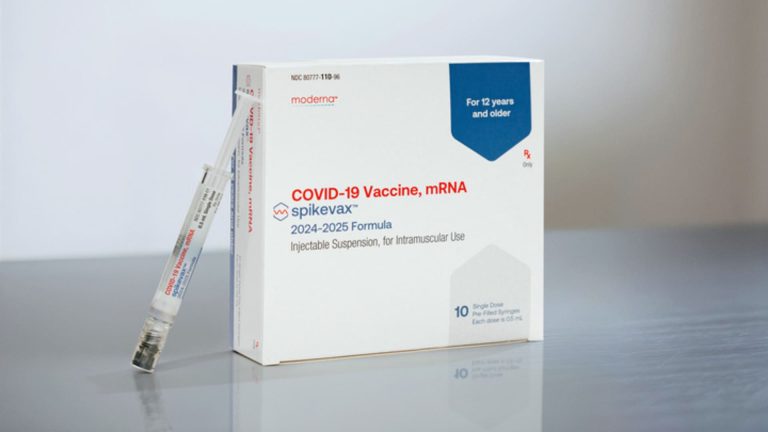
Moderna Covid-19 Vaccine mRNA 2024-2025 Formula.
Provided by: Moderna
A version of this article first appeared in CNBC's Healthy Returns newsletter, which delivers the latest healthcare news straight to your inbox. Subscribe here to receive future issues.
It's that time of year again, when a new round of COVID-19 vaccinations begins rolling out to Americans.
The US Food and Drug Administration last week authorized improved mRNA vaccines from Pfizer and Moderna amid a relative summer surge in virus infections. Here's what you need to know about how these vaccines are different from previous ones, who is eligible, and where you can get vaccinated.
What is the difference between these shots?
U.S. health officials have long told patients that COVID-19 vaccines need to be updated every year because the virus mutates into new strains that can evade the immunity people have built up from previous vaccinations or infections, similar to how the U.S. rolls out a new flu vaccine each year.
Now, the Pfizer and Moderna vaccines are designed to target a strain called KP.2, a descendant of the highly contagious Omicron variant JN.1 that began circulating widely in the U.S. earlier this year.
Although KP.2 was the predominant strain of the virus in May, as of August 17 it only accounts for about 3% of all infections in the United States, according to the most recent data from the Centers for Disease Control and Prevention (CDC).
Still, both Pfizer and Moderna say their new vaccines can generate a stronger immune response against other circulating variants, including KP.3, than last year's vaccine, which targeted the Omicron strain XBB.1.5.
KP.3 accounts for about 17% of cases in the U.S., while a related strain called KP.3.1.1 accounts for about 37% of cases, according to CDC data.
“The good news is that the improved vaccines are a very good match for the KP.3 family of viruses that continues to become dominant,” CDC Director Mandy Cohen said at a press conference Friday.
Who is eligible?
The CDC recommends one dose of the COVID-19 vaccine for everyone 6 months of age and older.
To maximize protection, people should wait at least two to three months after their last COVID-19 vaccination or infection before getting the latest vaccine, Dr. Peter Marks, director of the FDA's Center for Biologics Evaluation and Research, told NPR last week.
Health officials also stress the importance of continuing to get vaccinated against COVID-19 among people at high risk of infection, including those over 65 and those who are immunocompromised or have serious medical conditions.
When will vaccinations be available?
Following last week's approval, both Pfizer and Moderna said they expect the new vaccines to be available in pharmacies, hospitals and clinics across the U.S. “in the coming days.”
Walgreens said in a statement Thursday that patients can now make appointments to receive the vaccine at its stores nationwide. The company said appointments for people 12 and older will open on Sept. 6.
Meanwhile, CVS's online vaccine scheduling system is accepting appointments as early as Wednesday, while Rite Aid's system is accepting appointments for early September.
The CDC plans to relaunch the appointment finder system once vaccines become more widely available.
When should I get vaccinated?
The FDA's Marks told NPR that the variants targeted by the newest vaccines are “pretty close” to the strains currently circulating in the U.S., so people will likely be vaccinated “as quickly as possible.”
But people who want to get the most protection from vaccination in preparation for a winter COVID-19 surge or the holiday season may want to consider waiting until September or October, he said.
“Getting vaccinated in September, early October seems like a pretty reasonable way to maintain protection through December and January,” Marks told the outlet. “It's not like it suddenly becomes ineffective. It's not like it suddenly becomes ineffective in three or four months. It's just that your immunity wanes over time.”
Can I get it for free?
Most private insurance plans, as well as the federal Medicare and Medicaid programs, cover the cost of COVID vaccinations.
Children can also get the shots for free through a federally funded program called Vaccines for Kids.
Meanwhile, the CDC's Bridge Access Program, designed to provide free COVID-19 vaccinations to underinsured or uninsured Americans, is not scheduled to resume this year.
But Dr. Demetre Daskalakis, director of the CDC's National Center for Immunization and Respiratory Diseases, said at a press conference last week that the CDC has set aside $62 million in funding for state and local vaccination programs to cover the costs of COVID-19 vaccines for uninsured and underinsured adults.
Can I get the Novavax vaccine?
Novavax has applied for approval of a new protein-based vaccine targeting JN.1, and the company says its vaccine should protect against the strain's descendants, including KP.2.3, KP.3, KP.3.1.1 and LB.1.
Novavax said in a statement last week that it is working “productively” with the FDA as the agency completes its review. Novavax expects its vaccine to receive authorization in time for the peak U.S. vaccination season.
If you have any tips, suggestions, story ideas or data, please feel free to send them to Annika at [email protected].
Healthcare Tech Update: CNBC tests Dexcom's new CGM Stelo
Jack Silva | SOPA Images | LightRocket | Getty Images
Earlier this month, I began testing a new continuous glucose monitor from diabetes management company Dexcom. Called Stelo, it's the company's first product that can be purchased over the counter without a prescription.
A continuous glucose monitor (CGM) is a small sensor that is attached to the skin and measures blood glucose levels in real time. Glucose is a type of sugar obtained from carbohydrates and is the body's main source of energy.
Blood sugar levels fluctuate in everyone's body, but over time, high blood sugar levels can lead to serious health issues like diabetes, heart disease, kidney disease, etc. CGMs are typically prescribed to people with diabetes to monitor their blood sugar levels and alert them to any emergencies.
Stelo is designed primarily for adults with prediabetes or type 2 diabetes who aren't using insulin, but can also be used by people without either condition. The device went on sale in the U.S. on Monday after receiving Food and Drug Administration approval in March.
Users can purchase a one-month supply of Stelo online for $99 or sign up for a recurring subscription for $89 per month. Patients can also pay using their flexible spending account or health savings account, Dexcom said. Dexcom has partnered with Amazon for delivery of Stelo.
I've been using the sensor for a few weeks now and have learned a lot from it already, making it a great product to try out when it comes to understanding your blood glucose data.
When the sensor arrives at your home, everything you need is in the box: First, put the sensor on your arm and pair it with the Stelo app.
There's no need to worry, as the app walks you through the process in detail. I cleaned the underside of my right arm, placed the Dexcom applicator there, pressed the button, and the sensor was instantly attached. The applicator has a tiny needle in it, which can be a bit scary, but I didn't feel a thing.
The CGM connects to the Stelo app via Bluetooth and takes about 30 minutes to warm up.
The first time I got to this step, I ran into a few issues. Once the device warmed up, I got an error message that read “minor sensor issue.” I was instructed not to remove the CGM and was told the issue would resolve within a maximum of three hours. I left it on for the rest of the day, but by evening I noticed some light bleeding around the sensor.
I decided to remove the CGM, which you can do by peeling it off like a sticker. I tried again with a new sensor on the other arm, and it warmed up and worked fine. No more bleeding issues. If you have any issues using the Stelo, you can message the chat feature on the website to ask questions and get a replacement if needed.
Overall, I found the sensor easy to wear. It's waterproof and lasts 15 days on a single use (a new record for Dexcom). It's gray, about the size of a quarter, and about half an inch thick. I felt like I could wear anything over it, although it did occasionally get caught when I was wearing long sleeves. I didn't even notice it when I was sleeping.
I also found the Stelo app interface easy to use, and I think Dexcom does a good job of presenting the data in a way that doesn't feel overwhelming or confusing.
The Stelo homepage displays your latest blood glucose readings, updated every 15 minutes. It also shows a graph of your daily readings. The graph includes a green shaded area that indicates your “target range,” which is the range Dexcom recommends users keep their blood glucose levels within, based on existing medical standards.
A tab on the side of the homepage is the “Events” page, where you can log meals, activity, finger sticks (another way to measure blood sugar), and other notes. You don't need to log every little detail of your day, but Jake Leach, Dexcom's chief operating officer, says it's important to record when your blood sugar spikes.
A blood sugar spike occurs when the amount of sugar in your bloodstream increases and then decreases rapidly, which often happens after a meal. Stelo notifies you when you experience a noticeable blood sugar spike and records it to help you reflect on what caused it, Leach says.
If you're new to CGM, be sure to read the articles in the Learn tab of the app. They're short and easy to understand, explaining concepts like what glucose is, what affects it, and why it's important.
After just a few weeks of using the Stelo, I've learned a lot about how my body responds to food and activity, and now that the technology is available to buy over the counter, I wouldn't be surprised if CGM becomes the next big wearable tech in the US.
If you have any tips, suggestions, story ideas or data, please feel free to send them to Ashley at [email protected].